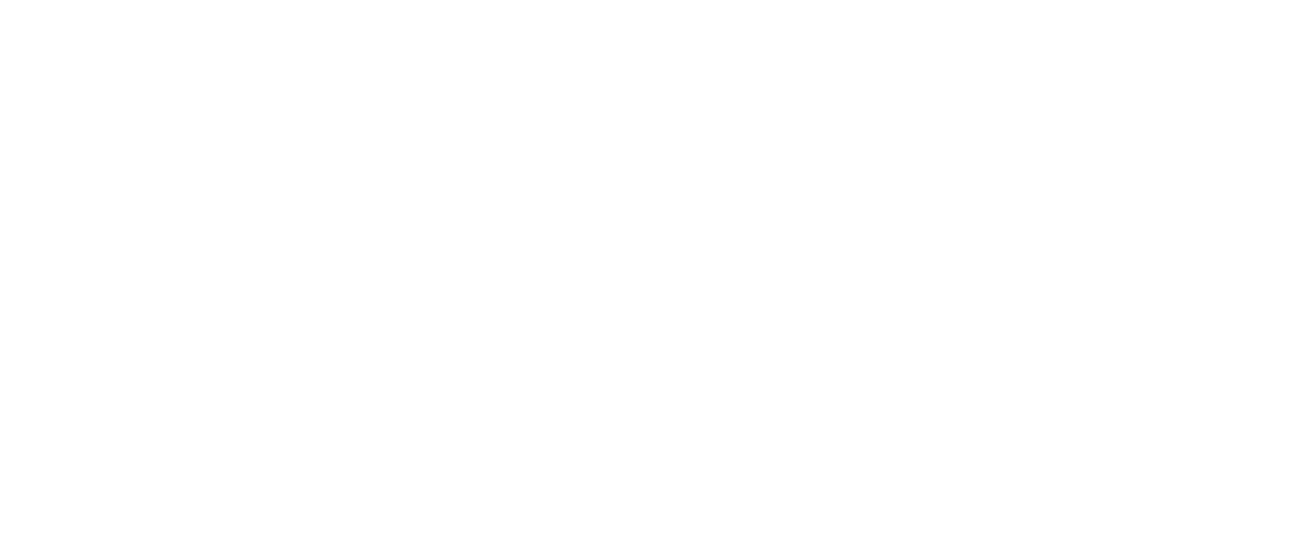
Easton has been fighting cancer for most of his twelve years. When he was 21 months old, he was constantly sick. His pediatrician noticed that his sickness was abnormal – he vomited more frequently in the mornings and while sitting in his car seat. A scan revealed a large tumor on Easton’s brain stem near the area that controls swallowing and nausea.
“The fact that Easton would get sick after being in his car seat made our pediatrician suspicious,” recalled his mother, Jill. “If the car seat hadn’t put pressure on the tumor, it might have taken longer to find.”

“We thought it was over,” said Jill. “We were told that if we had five years of clear scans, we wouldn’t have to worry about it again. Easton had four years of clear scans. But the cancer came back during the fifth year.”
Easton started treatment all over again in 2017 and experienced horrible side effects from the chemotherapy and radiation. Because the tumor grows around the area of the brain that controls swallowing, he has always had challenges eating. The awful mouth sores from his chemo caused him to be on a mostly liquid diet, and he had trouble maintaining weight.
In May 2022, Easton underwent a very risky surgery to try and remove the last part of the tumor. The surgery was unsuccessful. As he started recovering, Easton fell out of bed in the middle of the night. His parents rushed him to the emergency room, where doctors found that Easton’s brain was having a reaction to the glue that was used on his skull after surgery. He would need another risky brain surgery.
“This time, I felt like it was getting away from us and it was the beginning of the end,” said Jill. “He had been on some form of treatment for five years, and the tumor always found its way around it.”
But thanks to funding from CURE Childhood Cancer, Easton’s doctors have a new tool in their toolbox. CURE’s funds would pay for Easton’s tumor to be genetically mapped to see if his cancer involved any genetic mutations that could be targeted.
The genetic mapping revealed that a protein was feeding Easton’s tumor, causing it to grow. Doctors found an open clinical trial using a chemotherapy to inhibit this specific protein to prevent further tumor growth. Easton was immediately enrolled in the trial, and the results have been astounding. After four months, a scan showed that the inside of Easton’s tumor appeared to be dying. Three months later, the tumor is much smaller and is collapsing in on itself.
“The best news is that the tumor is dying. But also, he has no side effects. He can do the things a twelve-year-old should do while on this treatment,” shared Jill. “We’re still early in the process, but it has saved his life – at least at this point. I finally have hope for the first time in years. We are so encouraged and thankful to his doctors and to CURE for investing in precision medicine.”
Take the next step to support research that will help save kids with cancer… kids like Easton.









 “Trenton’s experience has shown us the huge need for less-toxic cancer treatments specifically tailored to kids and their growing bodies,” Ginger said. “Our family hopes that in the future, no other family will ever hear the heart-sinking words ‘Your child has cancer.’ But if that does happen, there will be hope – a hope of a cure and less toxic treatments tailored to kids that will allow them to be kids that grow into healthy adults.”
“Trenton’s experience has shown us the huge need for less-toxic cancer treatments specifically tailored to kids and their growing bodies,” Ginger said. “Our family hopes that in the future, no other family will ever hear the heart-sinking words ‘Your child has cancer.’ But if that does happen, there will be hope – a hope of a cure and less toxic treatments tailored to kids that will allow them to be kids that grow into healthy adults.”
 “Nicholas responded well to treatment in the beginning,” shared his mother, Cheryl. “But things went downhill fast. The nausea was relentless. He had pancreatitis from one chemo and had to have his gallbladder removed. Then he had an anaphylactic reaction to another drug. It was awful.”
“Nicholas responded well to treatment in the beginning,” shared his mother, Cheryl. “But things went downhill fast. The nausea was relentless. He had pancreatitis from one chemo and had to have his gallbladder removed. Then he had an anaphylactic reaction to another drug. It was awful.”
 Additionally, events that usually bring the childhood cancer community together have been canceled or held virtually. The Thomas family participated in 2021’s virtual Lauren’s Run and had a great time walking a 2k on the Silver Comet Trail (even after Zoe fell asleep.) This year, they are very much looking forward to the in-person Lauren’s Run & Picnic.
Additionally, events that usually bring the childhood cancer community together have been canceled or held virtually. The Thomas family participated in 2021’s virtual Lauren’s Run and had a great time walking a 2k on the Silver Comet Trail (even after Zoe fell asleep.) This year, they are very much looking forward to the in-person Lauren’s Run & Picnic.
 Further testing revealed that Chad was actually suffering from a different kind of leukemia, chronic myeloid leukemia (CML), which is very rare in children. The first task was to get his white blood cell count down so that he could travel home to the United States for treatment. This was only weeks after the September 11 bombing, so travel itself was no easy task. The family had to stay in England for another 45 days, but his counts finally allowed them to fly home.
Further testing revealed that Chad was actually suffering from a different kind of leukemia, chronic myeloid leukemia (CML), which is very rare in children. The first task was to get his white blood cell count down so that he could travel home to the United States for treatment. This was only weeks after the September 11 bombing, so travel itself was no easy task. The family had to stay in England for another 45 days, but his counts finally allowed them to fly home.


 During an eight-hour surgery, doctors removed the entire tumor and her right kidney. A biopsy confirmed it was a Wilms tumor and also showed it to have an anaplastic histology. This means that the cells’ nuclei are large and distorted, making the tumor harder to treat. Because of this finding, Jeneva had 30 weeks of chemotherapy and full stomach radiation after recovering from surgery.
During an eight-hour surgery, doctors removed the entire tumor and her right kidney. A biopsy confirmed it was a Wilms tumor and also showed it to have an anaplastic histology. This means that the cells’ nuclei are large and distorted, making the tumor harder to treat. Because of this finding, Jeneva had 30 weeks of chemotherapy and full stomach radiation after recovering from surgery.

 A few days later, he began to feel sick to his stomach. So they went to the emergency room, where a blood test revealed that Anderson had leukemia. He immediately started the standard treatment, which was scheduled to last three years.
A few days later, he began to feel sick to his stomach. So they went to the emergency room, where a blood test revealed that Anderson had leukemia. He immediately started the standard treatment, which was scheduled to last three years. “We were shocked when they said it was back,” Sally said. “Anderson had no symptoms. He was just getting routine labs.”
“We were shocked when they said it was back,” Sally said. “Anderson had no symptoms. He was just getting routine labs.”