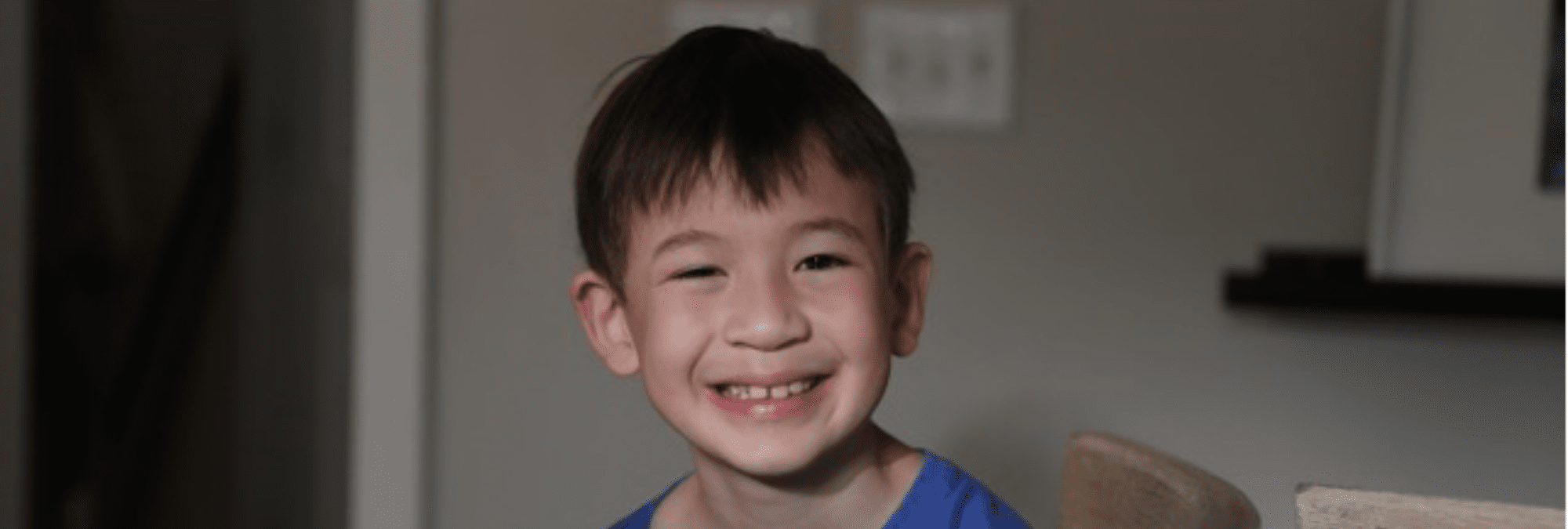
Edward Page’s cancer journey started on a Saturday morning in November 2017 while his soccer team was preparing to take on another team of four-year-olds. But instead of running onto the field, Edward didn’t want to play because his belly hurt. That day his life changed forever.
“In a few hours, we went from a stomachache to a cancer diagnosis,” said Edward’s father, Andrew. “Edward had a large mass in his abdomen that had already spread to his chest and bone marrow.”
Both of Edward’s parents are surgeons, and his father, Andrew, specializes in abdominal cancers. As a result, Andrew not only knew the prognosis of his son’s cancer, he also understood the value of molecular testing used in precision medicine.
“Precision medicine has changed the approach for difficult to manage cancers,” Andrew explained. “The concept of targeting pathways to stop tumor growth has changed the landscape for cancer treatment, as it can be more effective and less toxic than the standard chemotherapies. Precision medicine is like shooting cancer with a sniper, as opposed to shooting the whole patient with a shotgun.”
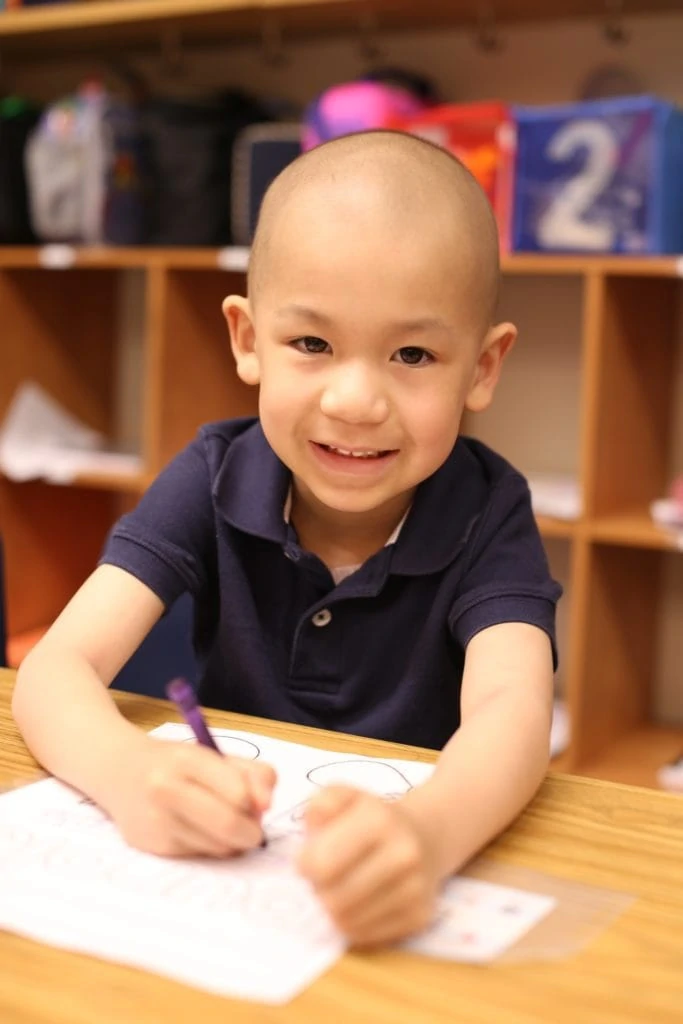
While precision medicine has been used to diagnose and treat adult cancers for years, it is very new to children. Thanks to CURE’s investment, Children’s Healthcare of Atlanta now boasts one of the nation’s leading precision medicine programs, offering this innovative treatment to children with cancer. After Edward completed years of standard treatment, which ultimately failed, he was enrolled in the program, and a sample of his tumor was sent for analysis.
“Genetic testing revealed that the relapsed cancer in his chest had a very specific mutation which was not present in the original tumor,” Andrew said. “Fortunately, the mutation has a drug that is proven to work against it.”
Watch Edward’s Story
Finally, this drug put Edward into remission. He is now cancer-free! Every day, Edward takes a pill which targets the cancer, ideally preventing recurrence. Today, he is healthy and strong and loves to spend his time outdoors. Since he had a kidney removed as part of his cancer treatment, he had to give up soccer. He now enjoys gardening and possesses a knowledge of plants well beyond that of most eight-year-olds. His family is so grateful for the opportunity to help him plant flowers.
“If it weren’t for the use of precision medicine, I am confident that Edward would not be with us today,” said Andrew. “The collaboration between Edward’s aggressive surgeon, Dr. Clifton, combined with Edward’s forward-thinking oncologist, Dr. Cash, unquestionably saved Edward’s life. Precision medicine is the way of the future, and our family is thankful for CURE’s investment in it.”
What is Precision Medicine?
In 2017, CURE made an unprecedented $4.5 million commitment to the Aflac Cancer Center of Children’s Healthcare of Atlanta to launch the Aflac Precision Medicine Program (APMP). With this award, the Aflac Cancer Center would become one of only a small handful of pediatric cancer centers nationwide able to offer this cutting-edge treatment approach to children with cancer.
An easy way to understand precision medicine is to think of it as “personalized medicine.” Although we know that every child is unique, today’s childhood cancer treatment does not take into account the genetic differences of each child. Rather, a child’s cancer is treated according to disease type. But often, children with the same type of cancer respond differently to the same treatment. A chemotherapy which is effective for some may fail altogether for others because of the genetic differences at play. That is where personalized medicine comes in.
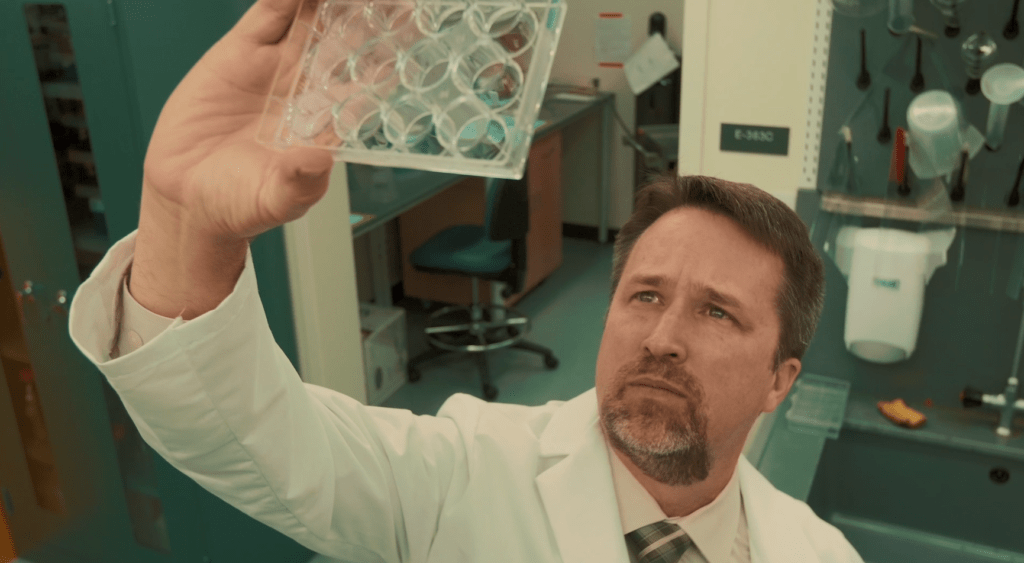
Over the past twenty years science has made incredible leaps in discovery by finding what is referred to as genetic barcodes – our DNA and RNA. We now understand what healthy cells look like and can often find triggers or markers in a tumor where something went wrong with a gene. By locating and isolating that problem and finding chemotherapies or other treatments proven effective against the genetic problem, doctors hope to improve survival while also minimizing exposures to toxic treatments which are not likely to work.
“There are really four outcomes when we look at genetic information taken from a child’s tumor,” explains Dr. Douglas Graham, Director of the Aflac Cancer Center. “The first is the perfect storm – we find a target that has a drug which is known to be effective against it and that drug is approved for children. We also may find a target with a matching drug that is not approved for children and would have to petition for access. The other options are not as optimistic. We may find a target with no drug known to work against it or we may find no target at all.”
The first step in the process is getting the child’s genetic information. Since July 2018, CURE has funded the genetic sequencing of more than 200 children with high risk or refractory cancers who would not have otherwise received the sequencing through another source.
For 85% of the children sequenced, their treatment was impacted by the genetic information obtained!
CURE Childhood Cancer remains determined that precision medicine is one of the most promising methods for improving survival rates in children. And we steadfastly believe that our children deserve the best and safest options available.